Submitted by San Juan Island Emergency Medical Service
Chances are you’ve had it happen to you a few times.
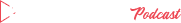
First a siren in the distance, and cars start pulling over. You copy them. Soon you see the lights and strain to see what’s happening. It’s an ambulance. You turn to the person next to you and say, “Someone is having a bad day.” Perhaps they turn onto your street, and an ambulance stops. A stretcher comes out.
For San Juan Island Emergency Medical Services that happened 1,184 times in 2019. It happened to 1,200 patients. Nationwide the trend continues towards an increase in calls, and that is mirrored here in Friday Harbor with a 9 percent increase over 2018. While it can be easy to forget that these statistics are real people or forget that every day this is happening to somebody, for our staff, each number represents real people that we see daily.
SJIEMS takes seriously its commitment to the public. We are funded through tax money, which combined with a series of grants and hybrid state-federal funding programs, enabled us in 2019 to move to a 24-7, 365 days a year staffing model. We do not charge coinsurance to island residents or landowners. EMTs are on-duty at all times. If you call, we will be there.
Some aid calls are critical, some are minor, but all taken seriously. Many are surprised to find out that only 75 percent of our calls resulted in a patient transport — about half of these transports were to PeaceHealth Peace Island Medical Center’s emergency department and about a quarter to air transit. Injuries are the most common patient complaint, with other main contenders being generalized weakness, abdominal pain, chest pain, and altered mental status.
About 60 percent of our calls were in the Town of Friday Harbor, and about 20 percent mid-island. In Town, it took an average of 7:17 minutes for the ambulance to arrive, and the further from town (generally) the longer a response takes. It now takes about 2 minutes for the ambulance to leave the station. A remarkable 66 percent of our patients were 55 or older. The busiest months are July-August, and the least busy was October.
All EMS agencies in the state of Washington are supervised by the Washington State Department of Health through a county-specific Medical Program Director. When Dr. Michael Sullivan retired from that position, Dr. Joshua Corsa has stepped into those duties for our county.
“Dr. Corsa has taken the bull by the horns and hit the ground running, getting to know and working with our responders,” said Interim EMS Chief Karl Kuetzing.
Staff reports a positive working relationship. The DOH also reviews and approves training plans.
Please remember to give our ambulances room. When possible, balancing patient safety and the safety of motorists and pedestrians, patients are transported without lights and sirens at a normal speed.
“Keep in mind that even if lights are not on, a patient may be inside the ambulance,” Kuetzing added. “If you do hear sirens or see flashing lights, they are for a purpose. Please clear the road and wait until the ambulance is safely away to start driving.”